
Codes and New Developments in HVAC for Healthcare
Hospitals and healthcare facilities have very specific heating and cooling needs – to maintain regulated temperature, humidity, and pressurization levels in operating rooms, intensive care units, and isolation rooms while simultaneously providing high levels of comfort in patient rooms and common areas.
Hosted by Amara Rozgus, Editor-in-Chief of Consulting-Specifying Engineers’ August webinar, HVAC: Hospitals and Healthcare Facilities Webcast, focused on addressing these concerns. Affiliated Engineers’ Jeremy Jones participated, discussing how variables within these facilities affect operating and life cycle costs, and how the changes in ASHRAE requirements, the FGI Guidelines, and various energy codes are driving project requirements.
The following summaries and elaborations were given by Jeremy.
ASHRAE Standards for HVAC
The delicate balance between maintaining ASHRAE standards and regulations while keeping patients and their families content and comfortable is a challenge. While ASHRAE doesn’t directly address the important considerations of patient comfort levels, these considerations can’t be lost while designers attempt to comply with the applicable codes. If the patients aren’t comfortable, the design has failed.
ASHRAE 90.1 governs the energy usage for buildings, along multiple HVAC compliance paths. The standard either allows the designer to work within an “energy budget” for the building, or provides a list of prescriptive requirements, governing aspects such as equipment efficiency, controls, damper leakage, insulation, fan power, and various energy recovery mandates.
ASHRAE Standard-170 specifies requirements for ventilation of healthcare facilities. It defines HVAC requirements for 81 common room types, pressure relationships, acceptable room temperature ranges, minimums for both total and ventilation air changes per hour, and spaces that must be directly exhausted. Detailed review of the footnotes, and adherence to all subsequent addenda, are required for full understanding and compliance.


Comparisons of HVAC Alternatives for Healthcare
The webinar compared multiple baseline HVAC system types commonly used in healthcare.
Constant Volume and VAV with Reheat. With a constant volume system, air is being sent into the room at a constant rate, resulting in a simple and predictable system to operate and maintain. This is highly energy inefficient, however, because it results in a constant need for simultaneous heating and cooling. Allowing these air quantities to fluctuate (with a VAV system) allows the design to more closely match the HVAC provided to the space with the actual room load. Simultaneous heating and cooling may still be required when actual room loads drop below code minimum air changes, but the result is still a significant energy savings when compared to a constant volume system.
Heat Recovery Chillers. Heat recovery chillers can be an energy-efficient strategy in healthcare, because they take advantage of any unavoidable instances of simultaneous heating and cooling by capturing waste heat from the cooling processes and harnessing them for the building’s heating needs. This waste heat would normally be rejected to the atmosphere.
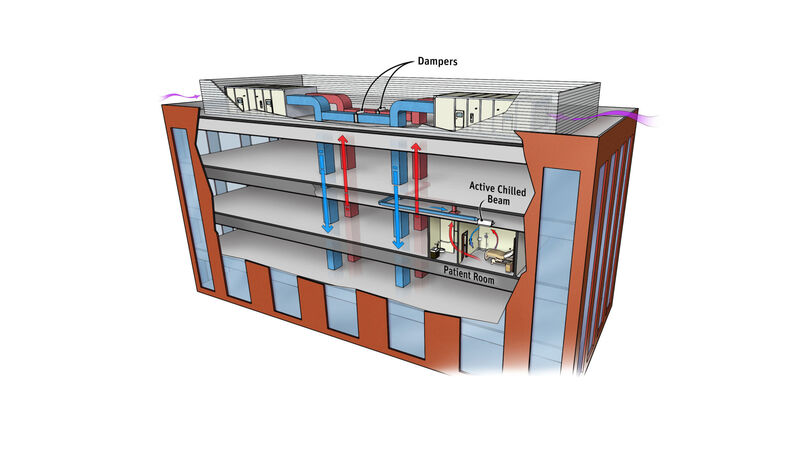

Active Chilled Beams. One very effective solution that is gaining traction in the healthcare industry is the use of active chilled beams in various spaces, including patient rooms. Water is a much more efficient heat transfer medium than air. This type of system allows only the ventilation air to be conditioned at the primary Air Handling System and distributed to the space. Local heating and cooling loads are satisfied by heating water and secondary chilled water at the space itself. Return air is recirculated within a given space, eliminating an entire duct system. Another benefit this system type provides is preventing cross-contamination between spaces (such as adjacent patient rooms).
Active chilled beams are applicable in most healthcare spaces where ASHRAE 170 does not prohibit the use of recirculating room devices. This makes them appropriate for patient rooms ancillary spaces, but clearly not operating rooms or isolation rooms.
Many other system types were discussed. See the linked webinar for a full explanation.
AEI Helps Moses Cone Hospital
In one of our new construction projects, Moses Cone Hospital’s North Tower Expansion, replaced the existing CEP, replaced air handling units across the existing campus, and included multiple energy conservation methods within the expansion itself. The result was a great improvement in energy efficiency campus wide. The North Tower was the first project to utilize active chilled beams in patient care areas. They were installed in 93 patient rooms. When compared to a traditional VAV system, the chilled beam system reduced overall ductwork (by weight) by 32%, making the options essentially cost-neutral. Temperature complaints saw a 431% improvement, when compared with the patient rooms in the existing hospital over the 14 months following occupancy.
How did they do this?
In spaces where active chilled beams are clearly not applicable, such as operating rooms, a VAV system with precision air terminals system is employed on both the supply and the return. While return air control is not a code requirement, it allows confidence that proper pressurization can be maintained at varying load conditions, and when the ventilation rate is set back during an unoccupied mode.
While opponents of active chilled beams will cite condensation potential as a reason to be nervous, our project has had no condensation events in the 6 years it has been in operation. A secondary chilled water system was created, which sends an elevated supply water temperature to the beams. Since we are constantly measuring space dewpoint, this secondary temperature can be reset to keep the surface temperature of the beams several degrees away from a condensation condition. While beam manufacturers have developed drain pan options to contain any potential condensation event, we definitely do not see them being beneficial or necessary with proper controls.
There is a perception, among some, that the recirculation inherent in an active chilled beam’s function could increase the risk of hospital acquired infections. Conversely, the fact that the system is a 100% outside air system, and that recirculation occurs only at the individual room level, a patient room served by an active chilled beam prevents cross-contamination between rooms. The North Tower had inherently better access to other infection prevention strategies, most notably handwashing, than the existing campus. The result is a space that performs better in every infection metric, when compared to the same population in the existing hospital. While we would never claim that chilled beams reduce infections, our gathered data certainly does not support the notion of them leading to an infection risk.
The move towards the implementation of active chilled beam in healthcare facilities is a beneficial yet challenging task. It does take careful consideration of dewpoint control, latent loads, and intermediate AHU temperatures. The utilization of this technology on this project has resulted in an increase in energy efficiency and patient satisfaction, and cleaner spaces than ever before. The data we have gathered in the years since occupancy is helping to prove these outcomes to educate the entire industry.